I felt good enough to lead worship at Redemption Church this morning. This was a big step for me for a number of reasons. First of all, I am lately bored out of my mind, with the same old routine going on most days: lots of ice, elevation, TV, and sitting around. I am normally a busy guy. So now that I have my mental faculties back to normal, not being busy is quite unpleasant. It was good to get back to doing something I love – playing guitar, singing, and leading others in worship.
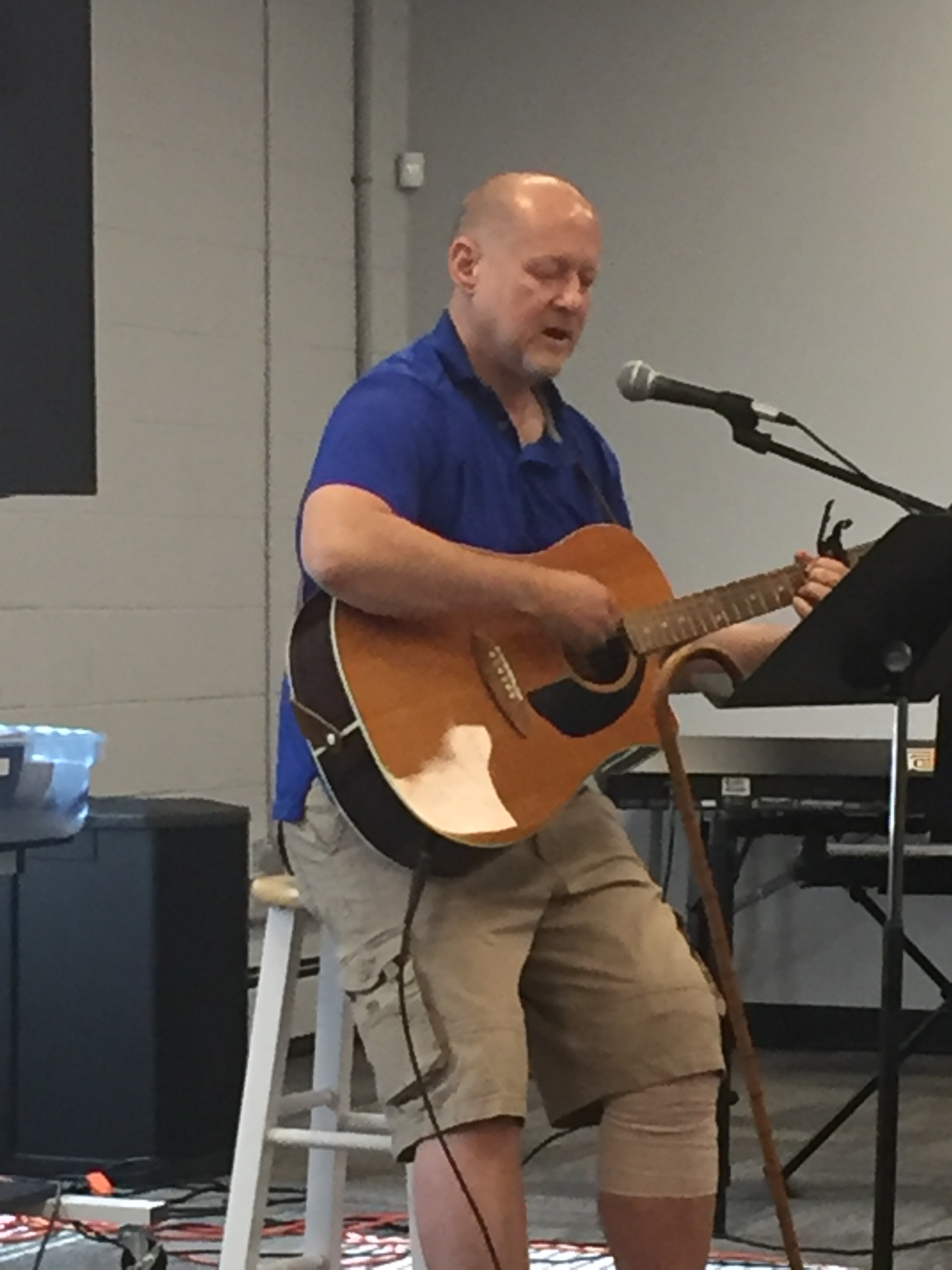
I have found that I must understand my limitations at this point. I can do something for an hour or two, then my knee begins to feel heavy and swollen, forcing me to elevate and ice, in order to feel comfortable again. I then feel surprisingly exhausted, since I really haven’t done all that much. I figure this is still a remnant of the surgery trauma on my body. My work at church this morning fit within those limitations.
Most of the energy during physical therapy at this stage is devoted to bending my knee in an attempt to develop normal flexion. I was at 111 degrees flexion at the end of last week. I do not know if that is good, bad, or normal. But everyone who worked with me seemed encouraged.
One of the things done at the beginning of a therapy session is work on a stationary bicycle. Initially, you are just warming up the knee and bending it at a level at which you are comfortable, since the amount of motion of the leg is controlled by the foot on the other pedal. During my last session, I had just begun working on the bicycle when a man at least ten years my senior sat down at a nearby bike and began pedaling vigorously. He saw me watching him and asked when I had my surgery. “June 7th,” I answered. “Same here,” he said. I felt a little twinge of jealousy, which was probably good for me, because I felt challenged to push myself a bit. I found that after a couple of minutes of concentration that I was able to pedal all 360 degrees. Progress!
I am at the end of week four. My surgeon stated that I would feel some sense of normalcy after six weeks. So I feel confident about where I am in the process of healing and rehabilitation. I anticipate substantial progress over the next two weeks!